Medical science has made extraordinary progress over the last few decades, with achievements that have led to an increase in general life expectancy and quality of life. Today, afflictions such as cancer, severe heart failure, polio, or tuberculosis have modern and effective treatments.
It is only fair to add vaccines to the impressive list of today’s modern medical solutions—pacemakers or brain stimulants, organ transplants, dialysis, prostheses, insulin, or levodopa (L-DOPA)—the list could go on. The World Health Organization estimates that about 2-3 million lives are saved each year by vaccination. It is also estimated that in the 40 years (1978-2018) since the eradication of smallpox (in 1977), approximately 200 million deaths that smallpox could have claimed worldwide have been prevented.[1]
What is the effectiveness of the COVID-19 vaccines? Why isn’t it 100%?
From time immemorial, both the medical world and patients, the beneficiaries of the medicine, have feverishly sought miraculous cures: maximum effectiveness, no side effects, low costs. This ideal is not only present in the medical field. You probably remember the ads for cars with a 10-year warranty. Or the windows with 50 years of durability guaranteed. The efficacy web does not bypass vaccination either. We are all waiting for the ideal vaccine, 100% effective and without side effects, right?
Vaccine efficacy and effectiveness
Let’s analyse two nuances. Although synonymous, efficacy and effectiveness will be used in different ways in this article, for scholastic reasons.
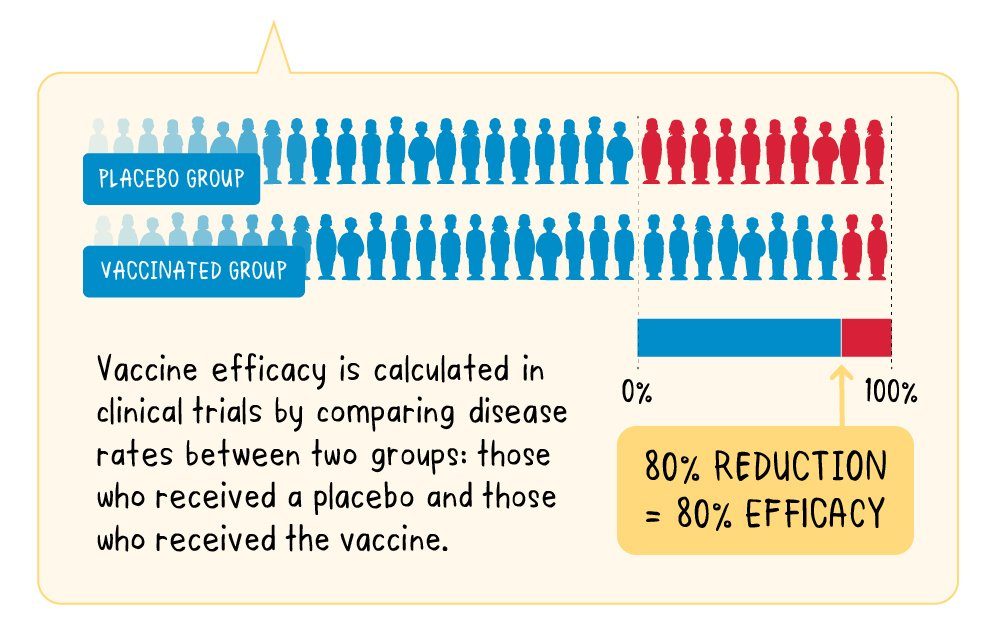
We define the efficacy of a vaccine as the percentage decrease in the number of sick people in a vaccinated group of people, compared to an unvaccinated (receiving placebo) group of people, in optimal conditions, meaning in a controlled clinical trial.
“Let’s imagine a vaccine with a proven efficacy of 80%. In practice, this means that—out of the people in the clinical trial—those who received the vaccine were at an 80% lower risk of developing disease than the group who received the placebo.” Therefore, 80% efficacy does not mean that 20% of the vaccinated group will become ill, but that the number of infections in the vaccinated group is 80% lower than the number of infections in the unvaccinated group.
 Source: H. Shaw Warren, Claude Leclerc, Adjuvants, Encyclopaedia of Immunology, ed. second, 1998, pp. 36-39.
Source: H. Shaw Warren, Claude Leclerc, Adjuvants, Encyclopaedia of Immunology, ed. second, 1998, pp. 36-39.
COVID-19 vaccines effectiveness
On the other hand, in this article, the effectiveness of a vaccine refers to the ability of a vaccine to prevent disease in the real world. The effectiveness is thus influenced both by elements related to the human factor (age, associated diseases/comorbidities, previous exposure to the virus, time elapsed since vaccination) and by the characteristics of the vaccine (whether it is a live-attenuated or inactivated virus vaccine, the mode and conditions required for its transportation, the addition of an adjuvant, etc.). For example, in 1925, it was discovered that adding various substances such as metallic salts, oil, tapioca and pyogenic bacteria to vaccine preparations increased the antitoxic response to diphtheria and tetanus toxins.[2]
Although clinical trials aim to include a broad spectrum of people, as representative as possible (different ages, both genders, different ethnicities, and those with known medical conditions), real-world effectiveness may differ from the efficacy of a vaccine. That is because the effectiveness of vaccination cannot be accurately predicted in a much bigger and more variable population than that which was included in clinical trials.
COVID-19 vaccines’ effectiveness over time
A study that tracked the experiences of 3,436,957 employees in the health field between December 2020 and August 2021 showed that the protection against coronavirus infection obtained by vaccination with BNT162b2 (Pfizer BioNTech) seems to decrease when it comes to the delta variant, from 90% in the first month after complete vaccination, to 53% four months after immunization. For the non-delta variants, the figures are better: from 97% in the first month to 67% after 4 to 5 months.
However, the effectiveness of the vaccine against infection requiring hospitalization remained high for the delta variant, regardless of age: 93% after 6 months. An important conclusion of this study is that the decrease in the protection offered by the vaccine is due to the decline in the body’s immune response that happens over time, and not the emergence of a new viral strain such as the delta. Hence the idea of the third dose (booster).
What needs to be emphasized is that the effectiveness of the vaccine remains high—despite the general impression—even in the case of new strains with higher transmissibility.
Some comparisons with other infectious diseases: influenza, tuberculosis, hepatitis, and measles
Influenza: The effectiveness of influenza vaccination, although estimated by the World Health Organization at 70-90% (2012), has recently been questioned. Although these percentages may be real in children vaccinated with an attenuated virus vaccine, the situation is different for inactivated virus vaccines at any age. Two recent meta-analyses report an effectiveness of 59%. In Australia, in 2010-2012, the vaccine protection against the AH3N2 flu virus did not reach 50%, being particularly weak in the elderly.
Tuberculosis is a major cause of death worldwide, being the leading cause of death from infectious diseases. An estimated 2 billion people are currently infected and mortality is just under 2 million a year. There is a vaccine, designed almost 100 years ago, which, although providing good protection against serious forms of the disease in children, is much less effective in adults. It is believed that the tuberculosis vaccine, known as Bacillus Calmette-Guérin (BCG) reduces the risk of infection by only 20%!
Hepatitis B: In this case, we have better news, as shown by the data: the effectiveness of the vaccine against hepatitis B viral infection has been evaluated in various studies at 95%. The decrease in the risk of acute infection is estimated at 85%.
Measles: The measles vaccine is also considered a truly effective vaccine because it reduces the risk of infection by over 95%.
Effectiveness of the existing COVID-19 vaccines in Europe
A comparison between the types of vaccines used to prevent SARS-CoV2 virus infection in Europe is also useful. Thus, from a comprehensive analysis published on the website of Mayo Clinic on November 5, 2021, we can isolate the aspects regarding the observed effectiveness of the Pfizer BioNTech, Moderna and Janssen/Johnson & Johnson vaccines:
Pfizer BioNTech (mRNA-based): 91% effectiveness in preventing symptomatic COVID-19 infection in people over 16; at least 89% effectiveness in the prevention of symptomatic infection in people with comorbidities, such as diabetes and obesity; 100% effectiveness in children between 12 and 15 years old; 91% effectiveness in children 5-11 years; protects against severe forms of the disease caused by various viral strains.
Moderna (mRNA-based): 94% effectiveness in preventing symptomatic infection; greater than 90% effectiveness in preventing symptomatic infection in people with comorbidities such as diabetes and obesity; protects against severe forms of the disease caused by various viral strains.
Janssen/Johnson & Johnson (adenoviral vector-based): 66% effectiveness in preventing symptomatic infection; 85% effectiveness in preventing severe forms of the disease; seems to protect against severe forms of COVID-19 produced by various viral strains.
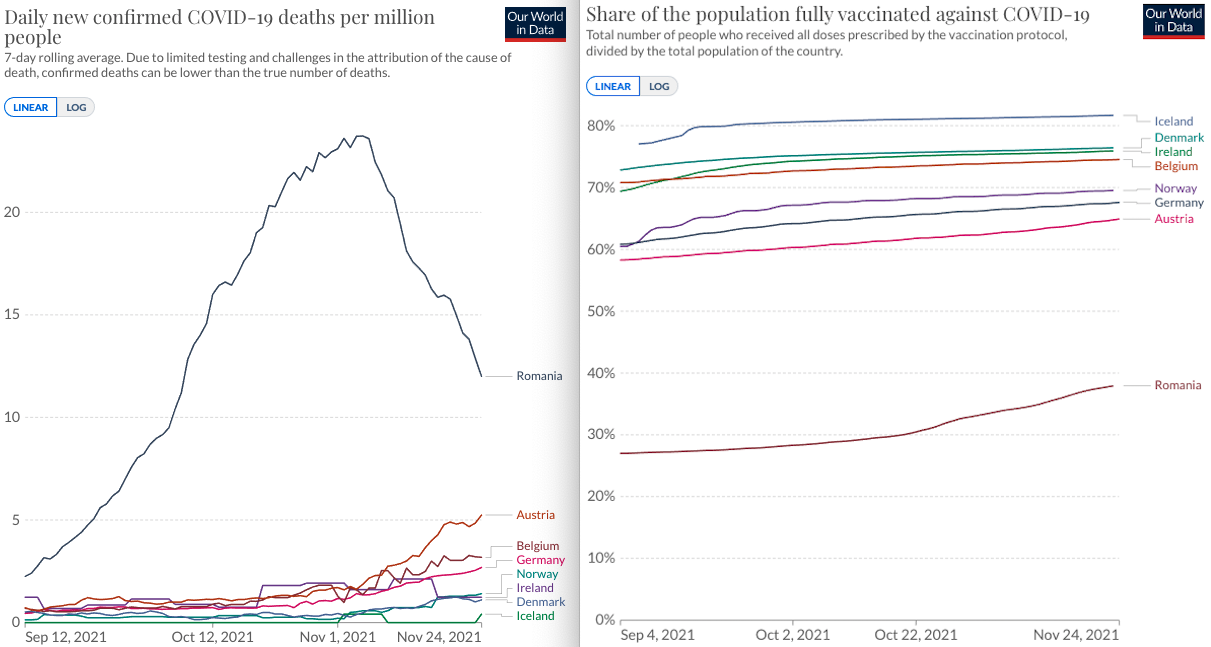
Comparative graph showing the inverse correlation between the share of the population fully vaccinated against COVID-19 and the average number of daily COVID-19 deaths per million inhabitants. (Source: Our World in Data)
Conclusion
In conclusion, although we are going through a difficult period from a medical point of view, we have this form of protection at our disposal: the vaccine against the SARS-CoV-2 virus. Although yet to be perfected, I consider it to be the best tool we have at the moment. May God give us wisdom!
Mihai Botezat, MD, is a primary care neurologist at Craiova County Emergency Clinical Hospital.



















