How long does the protection provided by the vaccine last? Should I have a booster shot after a while, or not?
The city of Manaus, located in the Brazilian part of the Amazon jungle, has a population of 2.2 million. In May 2020, a sharp rise in COVID-19 cases took place in Manaus, to the point that, according to some estimates, in October 2020, the cumulative incidence may have reached as high as 76%. Finding that the threshold of collective (or “herd”) immunity had been exceeded, the control measures and restrictions against COVID-19 infection have been relaxed. Yet, surprisingly, between December and January 2021, 7-8 months after the previous infections peak, the city that was believed to be protected was hit even harder than in the previous wave. Thus, on January 22, a record death toll was reached: 225 people. Several explanations have been suggested for this surprise in Manaus:
- A possible overestimation of the percentage of the population affected by the SARS-Cov-2 infection in 2020, and subsequent reassessments indicating a maximum value of 50%;
- Immunity to infection had reportedly begun to gradually decrease among the population since December 2020, after more and more individuals where exiting the 6 month period starting from their first exposure;
- The possibility that prior infection does not confer immunity for subsequent exposure to a new variant, if that variant is different enough from the previous one. In the case of Manaus, the second wave was generated by a variant with significant mutations in its spike protein;
- The specific variant for the second wave had a much higher transmissibility than the previous one, thus needing a higher threshold of immune coverage in the population (86% vs 70%).
Consequently, if we have been through a COVID episode, to what extent are we protected in the event of a new encounter with the virus, or one of its newer strains? How effective is natural immunity (the immunity developed by the body after the infection)?
Data from Great Britain (1.5% reinfection rate in the unvaccinated population, a proportion which is increasing with the appearance of the delta strain) and from the USA (5% reinfection rate after 3 months in the unvaccinated population, increasing to 50% after 17 months from the first infection episode), confirms that the high efficacy of post-infection antibodies decreases over time.
Moreover, in order to obtain natural immunity, one must first get through the first episode of infection with the SARS-Cov-2 virus. Unfortunately, what we discover from the experience of the city of Manaus is the fact that first infection is associated with an increased death risk or severe harm, especially for the elderly population and people with multiple associated diseases (85.7% of deaths occurred in people over 60, and 93.6% had associated comorbidities).
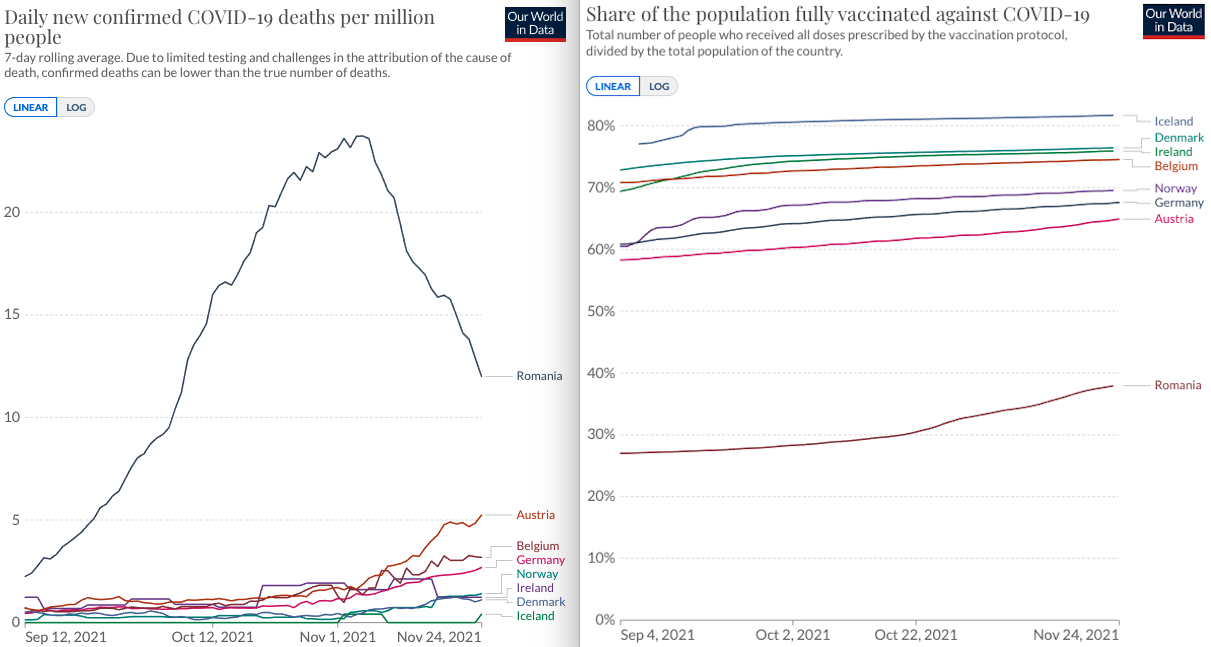
The good news is that protection obtained through complete vaccination is a solid guard against severe forms of the disease which require hospitalization, and against death.
Immunization against COVID-19 by vaccine decreases the risk of hospitalization
In a study conducted in the USA, on a group of almost 3.5 million people, the effectiveness of the vaccination with a full Pfizer dose was evaluated. Regarding the delta strain infection, the degree of protection decreased from 93%, one month after the second dose, to 53% after 4 months. However, the effectiveness of vaccination against infections requiring hospitalization remained around 93% after 6 months.
The results of studies such as this are confirmed by the current situation in Romania. An example is the Malaxa Hospital in Bucharest, a hospital that has been exclusively caring for patients with mild to moderate forms of COVID since the end of September 2021. In the Diabetes Department we have an average of 35 patients, out of which usually only one, maximum two, patients are vaccinated. The vaccinated develop mild forms of the disease, with a minimum need for oxygen therapy.
In contrast, with unvaccinated patients, although they are initially hospitalized with moderate lung damage and, in many cases, without needing oxygen supplementation, there are usually 3-5 patients, as young as 40 and 50, who develop severe cases that require the administration of aggressive oxygen therapy, with a high likelihood of being transferred to the ICU. For many patients this transfer is difficult to achieve due to the influx of severe cases, further limiting the space and resources that can be devoted to these patients.
Booster shots in COVID-19 immunization
Because the protective effect of the vaccine wanes over time, even to 50% after a period of 6 months after vaccination, it has been recommended that people have a third dose: the booster shot. The safety and efficacy of such an approach were assessed in a study conducted in Israel that included almost 1.5 million people. Although the follow-up period was very short (only 7 days) and the evaluation of the booster shot’s efficacy is still in its infancy, the results are encouraging: 93% efficacy in preventing hospitalization (29 infection cases compared to 231 in the control group), 92% efficacy in preventing severe forms of the disease and reduction by 81% of the number of deaths caused by the COVID-19 disease.
Given that the assessment of the safety and efficacy of the booster shot administration is still in its early stages, and even though preliminary data are encouraging, European organizations (European Center for Disease Prevention and Control, ECDC, and the European Medicines Agency, EMA) do not consider it urgent to administer a booster shot to the general population. They do, however, strongly recommend the administration of the booster shot/third dose to people with a weakened immune system (immunocompromised, transplant patients).
Booster doses may be considered by people between the ages of 18 and 55, if more than 6 months have passed since the full vaccination schedule. In conclusion, vaccination provides protection that declines over time, but it nevertheless remains useful for people who have not been through the disease, because it reduces the risk of severe infection or death. The third vaccine dose increases the level of protection, and the EMA encourages its administration, especially to those most likely to develop a severe form of COVID-19.
Laurenţiu-Daniel Roman is a resident doctor, specializing in diabetes, nutrition, and metabolic diseases, at the “Nicolae Malaxa” Hospital, Bucharest (dedicated COVID hospital).