What is in the COVID-19 vaccines? What remains in our system after each type of vaccine, and for how long?
There are many technologies applied in the production of SARS-CoV-2 vaccines. The four vaccines currently available in Europe are based on the following two different types:
mRNA vaccines
mRNA technology vaccines, namely the Comirnaty vaccine (Pfizer/BioNTech) and the Spikevax vaccine (Moderna), start from a relatively simple principle: SARS-CoV-2 is a virus whose nucleic acid is mRNA. This means that, when introduced into a cell, the nucleic acid is immediately used as a template for the production of viral proteins. The two mRNA vaccines work on the same principle. But unlike the coronavirus, whose RNA contains information needed to synthesize all viral proteins (having about 30,000 nucleotide bases), vaccines contain only the genetic information needed to synthesize a single protein—the spike protein (roughly about 3,700 nucleotide bases).
Once introduced into the body, mRNA vaccines rapidly transform into spike proteins. Studies in mice have shown that most of the vaccine’s messenger RNA remains in the muscle at the injection site. A significant percentage of mRNA reaches the surrounding lymph nodes, where it reaches a maximum level eight hours after inoculation. A much smaller amount of mRNA is distributed further into the body, to other tissues and organs.
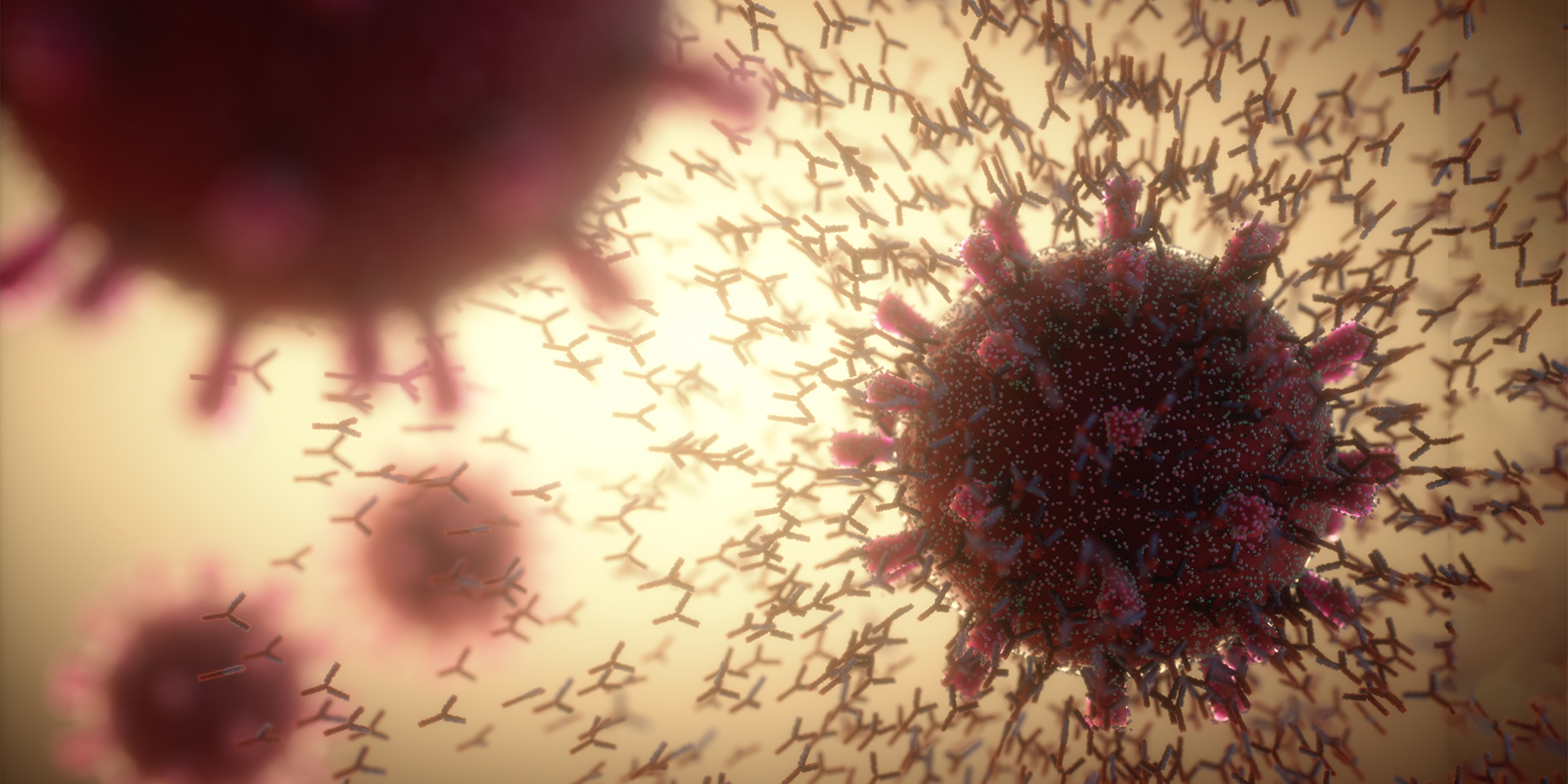
MRNA clustering in the lymph nodes is normal because it is at this level that immune cells and protective antibodies are produced. The lymph nodes are an important component of the lymphatic system, whose role is to eliminate excess fluid and waste from the body. A few days after vaccination, the entire amount of mRNA in the vaccine is fragmented and removed. After about 1-2 weeks, the spike proteins produced are eliminated as well, and only the protective antibodies and memory cells remain.
Adenoviral vector-based COVID-19 vaccines
Adenoviral vector-based COVID-19 vaccines—the Vaxzevria (AstraZeneca) vaccine and the Janssen (Johnson & Johnson) vaccine—use an adenovirus to deliver viral RNA. In this case, adenoviruses function like Trojan horses. They are completely harmless to humans because the structure of the vector has previously been stripped of all dangerous (infectious) components.
The main difference between Astra-Zeneca and Johnson & Johnson vaccines is that the former uses a chimpanzee adenovirus as a vector, while the latter uses a very rare human adenovirus, Ad26. It is imperative to use such rare viruses so that there is no immunity to the vector in the population (for example, the Russian Sputnik V vaccine uses an Ad5 as a vector, for which about 30% of the population already has antibodies, which explains the lower efficacy of this vaccine).
Once the vaccine is injected, the adenoviral vector delivers the recipe (template) to the cells for the production (synthesis) of the spike protein, after which it is destroyed and eliminated. Cells infected with the COVID-19 vaccine produce large amounts of spike protein and eliminate the vaccine in a few days or weeks. Synthesized spike proteins are recognized by the immune system, which consequently produces neutralizing antibodies.
Nucleic acids in mRNA vaccines do not enter the cell nucleus (where the DNA of the host is located), and adenoviral DNA cannot integrate into the nucleus either (a fact known for about 70 years), so there is no risk of the modification of our genes (human DNA) by COVID-19 vaccines.
Therefore, there is no cause for concern regarding the technologies used for the production of the COVID-19 vaccines available in Europe, or the interactions of these vaccines with the body.
By their nature, both types of vaccines minimize the proportion of additional elements in vaccines (neither uses adjuvants) which are often responsible for side effects. The body is presented with some simplified, incomplete, non-pathogenic variants of the virus, meant to protect and which, so far, have attained these goals.
Professor Cristian Apetrei, PhD, works in the Department of Infectious Diseases and Microbiology, School of Medicine and Doctoral School of Public Health, University of Pittsburgh, Pennsylvania, USA.