Early reports out of China showed that elderly people and the chronically ill were most vulnerable to Covid-19. Yet an alarming number of young people in the United States have been hospitalized with severe infections. According to the Centers for Disease Control and Prevention, nearly 40% of American Covid-19 patients who were hospitalized were under 55 – and 20% were between ages 20 and 44. And in rare cases, even children have died after falling ill with Covid-19. – The Guardian.
Is COVID-19 more dangerous for Caucasians, or in the West? Should we worry that the profile of the disease is different there? What do we know about how affected young people really are?
China
The first data available originated in China and, for a long time, these were the only data to which the rest of the world had access. At the end of February, the famous American medical journal JAMA published a summary of a report based on data from over 72,000 cases from the Center for Disease Prevention and Control in China. According to the summary, 3% of patients were 80 years of age or older, 87% were between 30 and 79 years old, and 8% of patients were young people between 20 and 30 years old. About 1% of infected people were between 10 and 19 years old, and another about 1% were children under 10 years old.
As for severity of cases, 81% were mild, 14% were severe and 5% were critical. Examination of deaths indicated that in most cases the death had occurred in elderly patients (a mortality rate of 14.8% in those over 80 years and 8% in those aged 70 to 79 years, while the mortality rate in the general population was only 2.3%). This indicates that, indeed, the elderly are much more likely to die from COVID-19 than younger people.
Other data from China (on smaller samples) are consistent in this respect. For example, of a series of 102 patients at a Wuhan hospital, patients ranged in age from 37 to 67, half under 54 and half over 54. Patients who survived were generally younger and they suffered from comorbidities in a smaller proportion.
A study published by a group of British researchers based on data from 3,665 cases of COVID-19 in China estimated hospitalization rates that would apply in the UK, taking into account the population structure there (and using an appropriate statistical methodology). Their estimate is that the following percentages would need hospital care: 0.04% of young people aged 10 to 19, 1% of people aged 20-30, 3.4% of those aged 30-39, 4.3% of those aged 40-49, 8.2% of those aged 50-59, 11.8% of those aged 60-69, 16.6% of patients aged 70-79 and 18.4% of those over 80 years old.
South Korea
A review of 54 COVID-19 deaths registered during the early onset of the pandemic in South Korea found the patients’ ages varied from 35 to 93 years, with a median of 75.5 years; in other words, half of the cases were over 75.5 years old, and half were under 75.5 years old. No patient under the age of 20 were among these first 54 victims, and there were two victims between the ages of 20 and 50. The fatality rate was certainly directly correlated with age: 0% between 0 and 20 years, 0.05% between 20 and 50 years, 0.77% between 50 and 70 years and 5.3% in patients over 70 years.
The conclusion of the article, published by the Korean Society of Infectious Diseases and the Korean Centers for Disease Prevention and Control, is that “clearly, patients over the age of 70 are more likely to die from COVID-19 infection than younger people, and men had higher fatality rates compared to women.”
Italy
Regarding the situation in Italy, in mid-March one of the first published studies reported data on 8,342 diagnosed patients, of whom 357 died. Half of the patients were over 65 years old and half were under 65 years old (almost two thirds of all cases were men). The distribution of cases diagnosed by age groups and mortality rate is shown in the graph below.
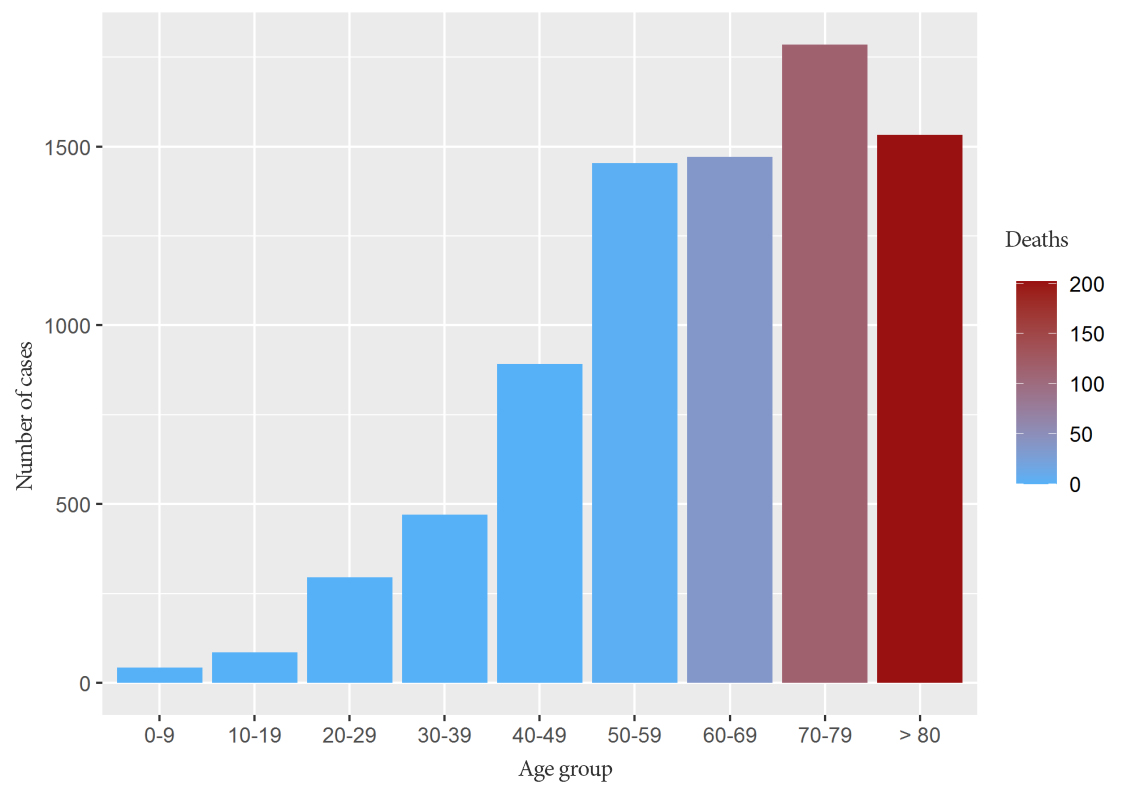
Of the total number of deaths, more than half (56%) were patients over the age of 80. Almost a third of all deaths occurred in patients aged 70 to 79 years, and about 10% in patients aged 60 to 69 years. Only 0.8% of the total deaths analysed in this sample were between 50 and 59 years old, with no deaths in patients below the age of 50.
A review of deaths in Italy, by age group, is very similar to that in the published sample to which we referred above. The only notable difference is that in the age group of 40-49 there is a small number of deaths (114 compared to over 12,000 recorded in those over 70), an even smaller number in those aged between 30 and and 39 years (30 cases), six deaths in patients aged 20 to 29 years and one death of a child under 10 years of age. Compared to the over 12,000 deaths registered in people over the age of 70, the 114 deaths in the 40-49 age group represent less than 1%, and the other age groups represent even less.
United States
Therefore, data from China, Korea and Italy all indicate a higher mortality the older the patient, and in patients under the age of 50 the mortality rate is quite low. Are things different in the United States, as the Guardian suggested?
The British publication based its claims on a report published by the Centers for Disease Prevention and Control (CDC), the official body in the United States (and one of the most reputable in the world). The report posted online on March 18 was subsequently corrected and officially dated March 26, 2020. According to this report, in mid-March, 4,226 cases of COVID-19 had been reported in the US. Of the 2,449 patients whose age was known at the time of the report, 6% were over 85 years old, 25% were between 65 and 84 years old, 18% were between 45 and 64 years old, and 29% were between 20 and 44 years; only 5% of cases had occurred in people under 19 years of age.
Although this does not indicate an excessively high proportion of infections in young people, this report does show a relatively high proportion (29% in those aged 20 to 44). However, as we already know, it is not the proportion of infected cases (people who have the virus) that should concern us, but the proportion of serious cases according to age. The CDC informed that, of the 121 patients who had been admitted to intensive care, 7% were adults over the age of 85, 46% were adults between the ages of 65 and 84, 36% were adults aged 45 to 64, and 12% were adults aged between 20 and 44 years. No intensive care hospitalizations had been reported in people under 19 years of age. Moreover, the analysis of death in people diagnosed with COVID-19 indicated that fatalities were highest among people over 85 years (10-27%), followed by those aged 65 to 84 years (3-11%), and between 55 and 64 years old (1-3%). Less than 1% of deaths were of people between the ages of 20 and 54 and no fatalities were reported in young people under 19 years of age.
Instead of conclusions
Data that was reviewed in different regions of the world agree in indicating that the risks associated with COVID-19 are directly related to age: the older the patients, the greater the risks. Conversely, the risk for young patients is relatively low. Very few deceased patients were registered under the age of 19, only a few under the age of 40 and even among those aged 41 to 59 the proportion of fatal cases is low.
Of course, these are probabilistic events described at the level of the analysed population samples. There may be small differences in different parts of the world, related not only to the polymorphisms in the patient’s body, to the known or as yet undiagnosed comorbidities of a patient, but also to the medical resources certain patients had access to.
The fact that young patients have a much, much lower probability of dying from COVID-19 infection does not mean that they should feel safe. This low probability of death for young people is higher than the probability of winning the lottery (which, as is well known, is negligible), but even in the lottery there are winners. Therefore, young people should not panic, but neither should they treat the problem with the indifference of “immortals” that the disease cannot reach. It’s not just about them, it’s also about others. To cherish those around you and to want to protect them is not a gesture of heroism, but a proof of humanity.
Robert Ancuceanu, PhD, is a professor in the Faculty of Pharmacy at the Carol Davila University of Medicine and Pharmacy in Bucharest, Romania.